Why home health care agencies struggle to play a significant part in reducing the $7.8B spent by payers on adverse drug event hospitalizations.
Continue reading5 Areas Your Home Health Agency May Want to Review to Enhance User Experience in 2024
Thriving Through Change in Home Health: A Comprehensive Guide
Change is an inherent part of the healthcare system, particularly in Home Health. Navigating annual alterations necessitates a proactive, strategic approach.
Continue readingPin the Tail on HCAHPS: Why Patient Experience is the Bullseye
Navigating the Home Health HCAHPS improvement can feel like your blindfolded at times and with the introduction of HHVPB its more important than ever.
Continue readingNavigating HCAHPS: From Patient Experience to Financial Success in Home Health Care
In the constantly changing home health landscape, understanding the nuances of the Home Health Care Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores is crucial for home health agencies. At the heart of this journey lies the differentiation between ‘patient experience’ and ‘patient satisfaction’, two factors that significantly influence the value-based purchasing (VBP) model.
Distinguishing Patient Experience from Patient Satisfaction
As explained by the Agency for Healthcare Quality and Research:
“The terms patient satisfaction and patient experience are often used interchangeably, but they are not the same thing. To assess patient experience, one must find out from patients whether something that should happen in a healthcare setting (such as clear communication with a provider) actually happened or how often it happened.
Satisfaction, on the other hand, is about whether a patient’s expectations about a health encounter were met. Two people who receive the exact same care, but who have different expectations for how that care is supposed to be delivered, can give different satisfaction ratings because of their different expectations.”
Below, we’ve selected a few HCAHPS survey questions to provide perspective on these two distinctions.
Q3: “Were you advised on how to safely organize your home when you began your home health care journey with this agency?”
Q4: “At the onset of your home health care, were you consulted about all the medications you were taking, both prescription and over-the-counter?”
Such questions focus on tangible interactions, spotlighting the patient’s experience. Conversely:
Q20: “On a scale from 0 to 10, where 10 represents the best possible care, how would you rate this agency’s home health providers?”
Q25: “Would you recommend this agency to family or friends seeking home health care?”
These questions aim to gauge the overall emotional response and the satisfaction levels patients have towards their care.
Here is a link to the HHCAHPS survey. Take a look and determine if you agree with our viewpoint that 16 out of the 19 questions, or 84% of the survey questions influencing an agency’s HHVBP scores, prompt patients to recall specific aspects of their home health care experience rather than measure their level of satisfaction.
The Financial Implications with Home Health Value Based-Purchasing (HHVBP)
In 2025, HCAHPS scores may influence up to 30% of the the home health value-based purchasing financial outcome. In the intensely competitive industry, these changes could have profound impacts on agencies Medicare reimbursement adjustments by up to 5%, either positively or negatively.
Implementation Change to Drive Success
Comprehensive Understanding of HCAHPS: Surveys indicate that while many home health executives understand the importance of HCAHPS, they believe only a few point-of-care clinicians genuinely grasp the HCAHPS survey. It’s vital to ensure your team fully comprehends each question and adjusts care strategies accordingly.
Revised Engagement Paradigms: Aim for patient engagements that are both meaningful and memorable. When patients recall experiences, the likelihood of them answering favorablely significantly increases.
Education & Skill Enhancement: Emphasizing the significance of HCAHPS scores to your staff is crucial to ensure they understand the substantial impact that patient experience has on the HCAHPS survey questions.
Integrating Proactive Feedback Mechanisms (Weekly calls as an example): Implementing a continuous feedback system that fosters ongoing patient engagement between in-home visits is essential. This system can involve activities like conducting weekly calls to gather updates, delivering standardized education regarding medication routines, emphasizing the significance of home safety, discussing upcoming schedules, and more. Such proactive measures are instrumental in averting the escalation of minor issues into significant challenges.
Upcoming ACHC Masterclass Webinar: Elevate Your Agency – Mastering HHVBP: Best Practices for Enhancing Quality of Care
For those eager to stay ahead and grasp impending changes, J’non Griffin, RN, SVP of Coding at SimiTree, will present a three-part ACHC masterclass webinar on HHVBP in September.
OASIS, Patient Engagement, and Expanded HHVBP Model – September 14, 2024
Reducing Hospitalizations with Care Management Protocols – September 21, 2024
Improving Patient Case Management to Increase HHCAHPS Scores – September 28, 2023
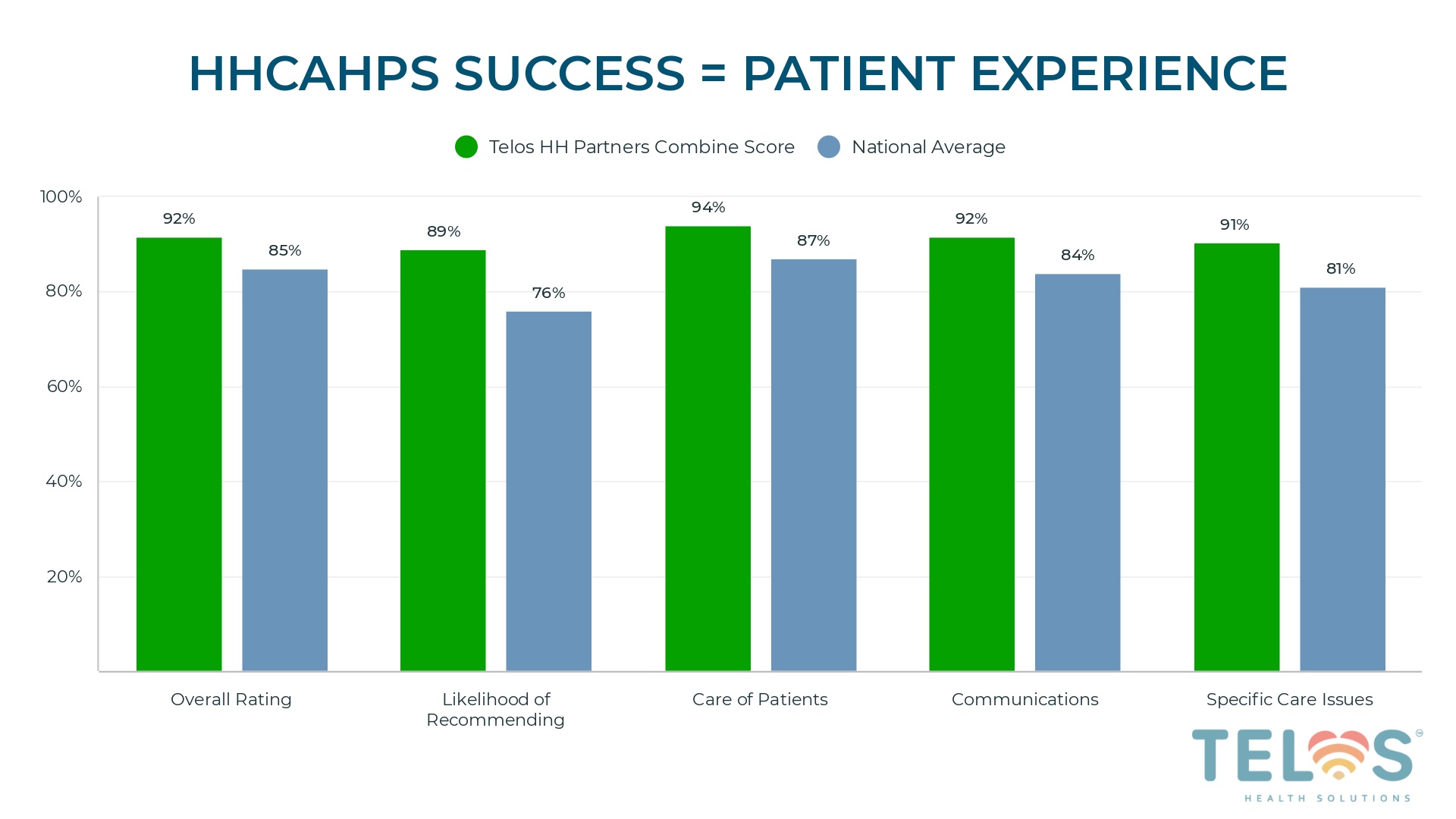
During the final session on September 28, 2023, Matthew Mulski, Co-founder of Telos Health, will join her to delve into the intricacies of HCAHPS questions and unpack the playbook Telos has used to assist its home health partners in outperforming the national average across all 5 HCAHPS measures, while also achieving a 4.61% hospitalization rate among patients actively engaged in their partners’ home health care navigation program (approximately 70% of patients receiving care from their home health partners as of mid-year 2023).
Remote Patient Monitoring vs. Care Navigation in Home Health: Our findings
In the quest to reduce hospitalizations, improve patient satisfaction (engagement), and better manage costs, home health owners/operators are recognizing the significance of implementing a virtual care strategy. In this process, most are evaluating two transformative tools: Remote Patient Monitoring (RPM) and proactive clinician-led telephonic engagements, which we term HH Care-Navigation.
They both aim to solve the patient engagement problem and provide providers with the patient insights between visits assisting them in tackling these complex challenges. Where the two differ specifically in the home health space is the infrastructure and logistics needed to operate a successful internal RPM program vs clinician led telephonic engagements.
Before delving into the details, let’s establish our internal definitions of RPM vs. Care Navigation and clarify that we’re not here to knock RPM. We are a RPM technology vendor and have worked with over 150 providers who’ve successfully established programs utilizing both our RPM and Care-Navigation solutions. It’s important to note that this article is primarily focused on the opportunities and challenges of home health providers serving patients for which there is currently not a reimbursement, such as Medicare and Medicare Advantage.
Definitions
Remote Patient Monitoring: We look to CMS’ definition of RPM, which involves the use of digital technologies to securely collect health data from patients in one location and transmit it electronically to providers in another location. This data can include vital signs, weight, blood pressure, blood sugar, pacemaker information, and more.
HH Care-Navigation: These checkpoints can be viewed as audio-only visits with a positive twist. Utilizing technology designed around the unique home health space, Care-Nav assists care teams in gathering updates on patient perceptions, providing standard of care information based on patient challenges, and capturing other valuable information that enable agencies to proactively address day-to-day challenges with a focused approach such as upcoming visit coordination, falls, medication adherence, shortness of breath, and more.
1. Cost of Scalability
Remote Patient Monitoring: Traditional home health RPM solution offerings often rely on physical equipment and internal staff to implement and monitor patients, which is obviously costly and typically hinders scalability due to budget constraints all home health agencies face.
HH Care-Navigation: In contrast, Care-Nav circumvents the reliance on expensive physical equipment, offering innovative technology solutions combined with outsourced clinicians responsible for engaging patients on behalf of the agency, making it possible to scale the program in a cost-effective manner for home health agencies. This empowers agencies to extend the benefits of virtual engagements to a wider patient population without adding an additional burden to their care teams or utilizing financial resources on equipment that might not be applicable for the agency’s entire patient census.
2. Equipment Logistics and Set-up
Remote Patient Monitoring: One of the primary challenges faced by home health agencies when implementing RPM revolves around logistical and educational requirements for clinical teams. Successful implementation requires thorough education of all care team members on the technical specifications of the equipment to ensure a positive patient experience. At one point, we shipped devices to patients’ homes for our home health clients, which sometimes resulted in added stress for their staff due to the fact that they had to send someone for an onsite visit or burdened them with coordinating a visit with the shipping date to ensure there were no patient setup issues. Even with solutions that don’t require a tablet or devices to be synced via Bluetooth, seniors deserve and need hands-on assistance with devices at times. The highest rate of success we’ve seen is with agencies that have a well-established and bought-in team that deploys devices in homes at the start of care, allowing monitoring to start immediately with devices that are cellularly embedded (automatically transmit upon patient use).
HH Care-Navigation: A Care-Nav program alleviates this by leveraging proactive clinician-led virtual engagements, where point-of-care clinicians only need to educate their patients and gain their buy-in. It’s akin to a personal check-in call (checkpoint) with patients that provides instant updates to care teams, allowing them to better understand the challenges their patients face between visits and offer improved assistance to help patients reach their care goals.
3. Technical Support
Remote Patient Monitoring: Technical issues with RPM devices can lead to patient frustration, and home health staff may lack the time or expertise to provide over-the-phone technical support. This may necessitate physical visits to troubleshoot problems and reduce patient frustration.
HH Care-Navigation: Care-Nav addresses this challenge by eliminating the need for physical equipment to capture patient-reported updates. Patients simply receive a call from the agency’s office number to provide updates, which are then automatically delivered to the appropriate members of the home health care teams. This streamlined process ensures reliable virtual technical support, enhancing patient satisfaction.
4. Success with Specific Patient Populations
Remote Patient Monitoring: RPM technology has shown remarkable success in managing specific patient populations, such as those with CHF or COPD, thanks to targeted monitoring and intervention strategies.
HH Care-Navigation: While RPM has shown outstanding results with patients who are willing and able to use equipment on a daily basis, Care-Nav aims to be a more comprehensive solution that can cater to diverse patient populations. It provides the opportunity for agencies to expand their monitoring initiatives to a broader range of patients, ultimately increasing the overall quality of care for all patients without losing opportunities to identify early intervention opportunities across unique and specific patient populations.
As the demand for virtual patient engagement in home health care continues to grow, both RPM and the Care-Nav program present valuable and positive solutions. RPM offers targeted monitoring for specific patient populations, but it comes with challenges related to installation, patient education, technical support, and costly physical equipment.
On the other hand, the Care-Nav program stands out by streamlining a scalable process that is capable of engaging all patients. It eliminates the need for in-person installations, offers reliable virtual support, and reduces costs associated with physical equipment and needed internal staff, similar to coding or oasis review outsourcing solutions. Moreover, Care-Nav’s versatility enables agencies to cater to a wider range of patient populations effectively, ensuring a positive impact on patient care.
Ultimately, the choice between RPM and HH Care-Nav depends on the specific needs and goals of your home health agency. For agencies that can make it financially feasible, we highly recommend launching a program that incorporates both solutions.
By understanding the key differences and advantages of each approach, we hope this helps you make an informed decision when the time comes to begin evaluating your virtual care strategy.
Use the calendar below to schedule a time with us to learn more about the technology or services we have designed to assist home health success in the value-based world.
Unraveling Patient Experience: The Intersection of Cost Efficiency and Patient Outcomes
Bridging the Home Health Quality-vs-Cost Gap: The Power Patient Engagement as a Service
Home health agencies find themselves in a delicate balancing act, as conflicting objectives create additional challenges for care teams. On one hand, they must prioritize quality outcomes to keep patients out of the hospital and mitigate the potential negative financial impact of HHVBP. On the other hand, they must optimize visit utilization to reduce care delivery costs ahead of impending reimbursement reductions in 2023. This intricate dance places significant pressure on agency leaders to navigate these competing demands effectively, all while avoiding an increase in workforce turnover.
Partnering with a Virtual Patient Engagement as a Service provider offers a solution for leaders to bridge the gap between quality care and visit utilization for clinicians. This collaboration extends the reach of the care team by providing patients with valuable clinician-led engagements between in-person visits. By leveraging this forward-thinking approach, the risk of burnout and reluctance towards new initiatives or responsibilities can be mitigated, empowering care teams to deliver exceptional care with more information while maintaining a balanced workload.
What is Virtual Patient Engagement as a Service
Virtual Patient Engagement as a Service is a resource for home health agencies to stay connected with and support their patients through meaningful clinician-led engagements that take place between in-person visits. By proactively engaging patients through virtual means, agencies can enhance their level of patient engagement without placing excessive burden on their existing clinician workforce. Patients are reached through phone calls initiated from the agency’s office number, allowing for additional education, updates, and more to be provided, all of which are then reported back to their care teams for further action and monitoring.
Benefits of Working With a Patient Engagement as a Service Partner
Virtual patient engagement services offer more than just virtual clinician and patient interactions. Providers like Telos employ clinicians who work as an extension of the agency’s care teams to deploy innovative technology and processes that provide actionable insights and capture information from patient and electronic health records. Care teams receive valuable updates regarding the patient’s progress and priorities after each virtual engagement, enabling them to make proactive decisions and adjustments to the care plan. This personalized approach helps deliver effective care while minimizing the number of in-person visits required.
The Importance of Clinician-led Engagements Between Visits
Regular clinician-led engagements play a crucial role in helping home health patients achieve their care goals and prevent hospital readmissions, ultimately leading to improved quality outcomes. These interactions are essential in delivering high-quality care. However, reducing the number of in-person visits presents a challenge for care teams, considering their deep understanding of the positive impact that regular interactions have on patients. Moreover, keeping patients out of the hospital is the primary performance metric by which their performance is evaluated.
Empowering Care Teams and Fostering Trust
A Patient Engagement services partner who is truly invested in their clients’ success should focus on helping them recognize both the financial and patient-centric impact they are assisting in making through quality insights and actionable data. This ultimately provides peace of mind to care teams in the field. This collaborative effort should further foster an internal agency culture of trust and understanding, where clinicians feel confident in navigating the balance between optimizing visit utilization and delivering high-quality care. This confidence stems from knowing that their patients receive continuous support, even when they are not physically present. Such empowerment enables care teams to be open-minded about operational adjustments and fulfill their mission of providing high-quality care within limited resources.
Before Committing to a Long Term Contract,
Ensure It Effectively Solves The Problem
While a patient engagement-as-a-service partnership is a solution that can offer a lot of potential benefits in solving complex problems at the clinician and patient level, we advise all our clients to ensure they have the flexibility to exit the contract if the partnership doesn’t meet their expectations. Even better, consider asking the provider if they are willing to share the risk by establishing pre-determined metrics and goals. This approach ensures that both parties are committed to achieving the desired outcomes and can make adjustments if needed.
Click above to review our Mid-year client performance metrics or contact us to learn more about how we partner with home health care agencies through a data-driven yet patient-centric approach.