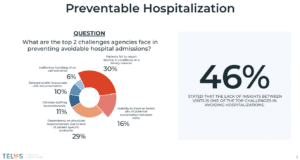
In the quest to reduce hospitalizations, improve patient satisfaction (engagement), and better manage costs, home health owners/operators are recognizing the significance of implementing a virtual care strategy. In this process, most are evaluating two transformative tools: Remote Patient Monitoring (RPM) and proactive clinician-led telephonic engagements, which we term HH Care-Navigation.
They both aim to solve the patient engagement problem and provide providers with the patient insights between visits assisting them in tackling these complex challenges. Where the two differ specifically in the home health space is the infrastructure and logistics needed to operate a successful internal RPM program vs clinician led telephonic engagements.
Before delving into the details, let’s establish our internal definitions of RPM vs. Care Navigation and clarify that we’re not here to knock RPM. We are a RPM technology vendor and have worked with over 150 providers who’ve successfully established programs utilizing both our RPM and Care-Navigation solutions. It’s important to note that this article is primarily focused on the opportunities and challenges of home health providers serving patients for which there is currently not a reimbursement, such as Medicare and Medicare Advantage.
Definitions
Remote Patient Monitoring: We look to CMS’ definition of RPM, which involves the use of digital technologies to securely collect health data from patients in one location and transmit it electronically to providers in another location. This data can include vital signs, weight, blood pressure, blood sugar, pacemaker information, and more.
HH Care-Navigation: These checkpoints can be viewed as audio-only visits with a positive twist. Utilizing technology designed around the unique home health space, Care-Nav assists care teams in gathering updates on patient perceptions, providing standard of care information based on patient challenges, and capturing other valuable information that enable agencies to proactively address day-to-day challenges with a focused approach such as upcoming visit coordination, falls, medication adherence, shortness of breath, and more.
1. Cost of Scalability
Remote Patient Monitoring: Traditional home health RPM solution offerings often rely on physical equipment and internal staff to implement and monitor patients, which is obviously costly and typically hinders scalability due to budget constraints all home health agencies face.
HH Care-Navigation: In contrast, Care-Nav circumvents the reliance on expensive physical equipment, offering innovative technology solutions combined with outsourced clinicians responsible for engaging patients on behalf of the agency, making it possible to scale the program in a cost-effective manner for home health agencies. This empowers agencies to extend the benefits of virtual engagements to a wider patient population without adding an additional burden to their care teams or utilizing financial resources on equipment that might not be applicable for the agency’s entire patient census.
2. Equipment Logistics and Set-up
Remote Patient Monitoring: One of the primary challenges faced by home health agencies when implementing RPM revolves around logistical and educational requirements for clinical teams. Successful implementation requires thorough education of all care team members on the technical specifications of the equipment to ensure a positive patient experience. At one point, we shipped devices to patients’ homes for our home health clients, which sometimes resulted in added stress for their staff due to the fact that they had to send someone for an onsite visit or burdened them with coordinating a visit with the shipping date to ensure there were no patient setup issues. Even with solutions that don’t require a tablet or devices to be synced via Bluetooth, seniors deserve and need hands-on assistance with devices at times. The highest rate of success we’ve seen is with agencies that have a well-established and bought-in team that deploys devices in homes at the start of care, allowing monitoring to start immediately with devices that are cellularly embedded (automatically transmit upon patient use).
HH Care-Navigation: A Care-Nav program alleviates this by leveraging proactive clinician-led virtual engagements, where point-of-care clinicians only need to educate their patients and gain their buy-in. It’s akin to a personal check-in call (checkpoint) with patients that provides instant updates to care teams, allowing them to better understand the challenges their patients face between visits and offer improved assistance to help patients reach their care goals.
3. Technical Support
Remote Patient Monitoring: Technical issues with RPM devices can lead to patient frustration, and home health staff may lack the time or expertise to provide over-the-phone technical support. This may necessitate physical visits to troubleshoot problems and reduce patient frustration.
HH Care-Navigation: Care-Nav addresses this challenge by eliminating the need for physical equipment to capture patient-reported updates. Patients simply receive a call from the agency’s office number to provide updates, which are then automatically delivered to the appropriate members of the home health care teams. This streamlined process ensures reliable virtual technical support, enhancing patient satisfaction.
4. Success with Specific Patient Populations
Remote Patient Monitoring: RPM technology has shown remarkable success in managing specific patient populations, such as those with CHF or COPD, thanks to targeted monitoring and intervention strategies.
HH Care-Navigation: While RPM has shown outstanding results with patients who are willing and able to use equipment on a daily basis, Care-Nav aims to be a more comprehensive solution that can cater to diverse patient populations. It provides the opportunity for agencies to expand their monitoring initiatives to a broader range of patients, ultimately increasing the overall quality of care for all patients without losing opportunities to identify early intervention opportunities across unique and specific patient populations.
As the demand for virtual patient engagement in home health care continues to grow, both RPM and the Care-Nav program present valuable and positive solutions. RPM offers targeted monitoring for specific patient populations, but it comes with challenges related to installation, patient education, technical support, and costly physical equipment.
On the other hand, the Care-Nav program stands out by streamlining a scalable process that is capable of engaging all patients. It eliminates the need for in-person installations, offers reliable virtual support, and reduces costs associated with physical equipment and needed internal staff, similar to coding or oasis review outsourcing solutions. Moreover, Care-Nav’s versatility enables agencies to cater to a wider range of patient populations effectively, ensuring a positive impact on patient care.
Ultimately, the choice between RPM and HH Care-Nav depends on the specific needs and goals of your home health agency. For agencies that can make it financially feasible, we highly recommend launching a program that incorporates both solutions.
By understanding the key differences and advantages of each approach, we hope this helps you make an informed decision when the time comes to begin evaluating your virtual care strategy.
Use the calendar below to schedule a time with us to learn more about the technology or services we have designed to assist home health success in the value-based world.