By Nora Silver, RN
The Home Health industry can be an overwhelming environment even for industry veterans. The sheer number of laws, rules, regulations, and standards that have to be met often cloud the view of the big picture. As if all the governance was not enough to keep industry leaders up at night, additionally there are STAR ratings, HHVBP, and Surveys that serve as the public report card of agency performance. These concerns are rounded out with financial challenges and staffing crises, creating the turbulent storm many agencies find themselves in.
Over the past 16 months, I’ve been able to step back and truly reflect on my 23 years of experience of living it at the agency level and be a part of building something that solved so many of the challenges our agency faced day in and out.
I’ve found various parallels across the high-performing agencies we work with at Telos Health Solutions, but the more I think about it, the more one universal aspect stands out: providers who set a unified goal around the end-user experience outperform the rest of the pack.
With that said, the end-user experience looks different for the different stakeholders, but there is a common denominator in which I feel all stakeholders desire. So, for owners/operators trying to rally their teams or putting new initiatives into place in 2024, I hope these 6 steps are helpful!
1: Define the Ultimate Goal
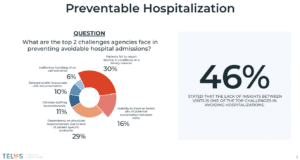
The ultimate goal of Home Health can be distilled into one simple idea: prevent unplanned hospital use and keep the patient at home.
2: Understand Stakeholder Influence
Understanding stakeholder influence is vital to effectively navigate from point A to point B in the most efficient manner. All too often in the home health arena, we as leaders can get caught up in the data points, which can lead us to lose sight of the levers that need to be pushed at the right time to achieve the desired outcome. For example, if we constantly educate our teams on the importance of outcomes from a payer perspective without providing insights or updates on how we, as leaders, are making changes to improve the clinical team’s day-to-day experience to assist them in achieving their set goals, it can often be lost on deaf ears.
3. Manage Risks Effectively
Identify potential obstacles to achieving the goal, including stakeholder engagement, injury prevention, safe medication use, symptom management, early detection of decline, infection control, maintaining functional stability, and ensuring adequate in-home support. Utilize the Medicare Conditions of Participation (CoPs) as a solid foundation for risk management and compliance. CoPs, such as patient rights, comprehensive assessment, and care planning and coordination, address patient-specific readmission risks. Additionally, consider integrating external strategies like virtual patient engagement programs, standardized staff education, and efficient OASIS/Plan of Care and coding practices to enhance success.
4. Build Momentum by Focusing on Small Wins
As clinicians, we’re typically set in our ways, and many of us abhor change. Combine that with the significant changes that have occurred in the industry over the last five years, and it’s become more challenging than ever to see the impact made through new initiatives. However, sometimes the only way to succeed is to be willing to think outside the box and embrace change. Instead of solely focusing on the end goal, which can often change, I’d recommend finding ways to shift your focus toward achieving small wins. A 1% improvement each day equates to a 36x improvement over the course of a year, so finding ways to set and accomplish small wins can go a long way in the grand scheme of things for a few reasons:
- It provides leaders with a means to showcase and praise teams for their accomplishments on a routine basis.
- It reduces friction when you need to adjust big-picture goals due to industry or market conditions.
5. Establish a Universal Scoreboard
Identify success indicators through STAR ratings and HHVBP, which combine OASIS data, claims data, and patient experience data, providing insights on performance from different perspectives. Use these public scores along with others provided by your solution vendors to pinpoint areas of strengths and weaknesses in achieving the ultimate goal of keeping patients at home. Furthermore, a scoreboard serves as a unified reference point for assessing your progress collectively as a team, enabling you to identify and address both technical (software/systems) and non-technical (process/communication) user experience roadblocks.
I truly believe that by focusing on the end-user experience and setting goals that strategically take stakeholder influence into account, home health agencies can navigate these challenges and thrive, ultimately providing better care and support for those who need it most in 2024.